General Questions
1. How do I make an appointment?
Currently, Mr Khazim holds clinics at the Spire Wellesley and Spire Hartwood private hospitals. If you prefer to be seen at the Wellesley hospital, please call 01702 445767, or book online here. To make an appointment at the Spire Hartswood hospital, please call 01277 232525, or book online here. Please note that Mr Khazim’s secretary is unable to make appointments, although she is of course happy to advise on his availability or answer any questions you may have before you book.
2. Do I need a referral to make an appointment?
Although Mr Khazim is happy to see you as self-referred, it is always best to have a referral from your GP. Ideally, the referral letter should include the condition for which you are being referred, any previous treatment you have had and any medication you are currently taking. Similarly, Mr Khazim will be happy to see you following referral by a colleague specialist, chiropractor, osteopath or physiotherapist.
To claim on your insurance, you may need a referral letter from your GP. It is recommended that you check beforehand that your insurance company will fund this appointment.
3. Is Mr Khazim an appropriate surgeon for me or my condition?
If you are unsure of the most appropriate specialist to see, you can ask your GP or your insurance company. Alternatively, you can contact Chrissie Nelson on telephone 07377 383225 (office days Mondays, Tuesdays and Thursdays), or info.secretary@spinalconsultant.co.uk to check if Mr Khazim is an appropriate specialist for your condition.
4. What do I bring to my initial consultation?
- Referral Letter (if possible)
- Copies of your X-rays, MRIs, CT scans and reports, blood tests and any other relevant information
- List of medications (if any)
5. How do I pay for consultations, scans or treatment?
When you book an appointment in Mr Khazim’s clinic, the hospital will take all relevant details from you, including details of your private health insurers, if relevant. Mr Khazim’s accounts office will invoice you if you are self-funding, or your insurance company, following each clinic appointment, and similarly the hospital will invoice for any scans or treatment you may have. Upon receipt of these invoices, any queries regarding consultation fees can be dealt with by the accounts office (01702 382314), or by the relevant hospital in the case of invoices for scans or treatment.
6. What is the Wellesley fixed price for surgical treatments?
When you attend Mr Khazim for an initial consultation, this may be followed with diagnostic tests or scans and a Follow-up appointment to review the scan results and discuss the management options. Initial and follow-up consultations, tests and scans (if required) are charged separately. Once you decide to proceed with an injection or surgical procedure self-funded, Mr Khazim will fill a booking form. The Wellesley hospital Bookings department will then contact you with a detailed fixed price for that procedure. This will cover all costs relating to this treatment from this point on. Your price is made up of your surgeon’s fee, anaesthetist fees, hospital fees (nursing, accommodation, food etc.) and the price of any necessary prosthesis. Your hospital fees cover everything you need for as long as you need to stay in hospital, so you don’t get any unexpected bills if for clinical reasons you need to stay for longer than planned.
Once you have left hospital, your fixed price covers one follow up consultation, and all standard post-operative care including take home drugs, the removal of stiches, dressing changes and all physiotherapy that your consultant advises you need. For additional peace of mind, should there be a clinical need for you to return to hospital within one month after treatment, to deal with complications of treatment, you will not receive an additional bill.
For more information, please call the Spire Wellesley hospital on 01702 447926 or visit their webiste - http://www.spirehealthcare.com/patient-information/paying-for-treatment/
7. Who can I contact for any post-treatment concerns?
Following your treatment and before your discharge from hospital after surgery, you will be given a point of contact 24 hours a day for any post-operative concern. This is usually the Wellesley Hospital ward phone number. The in-charge nurse will speak to you and if necessary you will be asked to attend the hospital to be reviewed by the Resident Medical Officer (RMO). If necessary, you may be admitted for review by Mr Khazim or a colleague designated consultant, or they will make you an appointment in the clinic as appropriate.
Post-Operative
1. Travelling in a car
On discharge you will generally go home in a car. To get into the car, push the passenger seat back as far as possible. Maintain an upright position for your spine whilst getting into the car and throughout the journey. You may find that holding onto the dashboard and doorframe assists you to lower yourself to the car seat. We advise that, whenever possible, to avoid being in a car for more than 20-30 minutes in the first 6 weeks. Thereafter, you can travel by car as tolerated, but whenever possible, it is advised to break up longer journeys with frequent stops (every 30 minutes), so you can get out and move around for few minutes.
2. Who can I contact for any post-treatment concerns?
Following your treatment and before your discharge from hospital after surgery, you will be given a point of contact 24 hours a day for any post-operative concern. This is usually the Wellesley Hospital ward phone number. The in-charge nurse will speak to you and if necessary you will be asked to attend the hospital to be reviewed by the Resident Medical Officer (RMO). If necessary, you may be admitted for review by Mr Khazim or a colleague designated consultant, or they will make you an appointment in the clinic as appropriate.
3. How long do I need time off from work after the surgery?
Recuperation after surgery varies depending on your general health, fitness, your preoperative condition and limitations and the particular operation you had. Most commonly, you will be able to start work from home (if possible) within 2 weeks. It may take up to 2-6 weeks before you resume work. If your work involves going by train or public transport, we advise you initially to avoid rush hours. If you are employed, most employers’ occupational health will agree with you a phased gradual return to work over a few to several weeks and avoiding heavy lifting, manual activities and repetitive pushing, pulling and twisting for weeks after resumption of work. You will be provided with a sick note certificate for the necessary time off work after surgery.
4. When can I resume driving after surgery?
It is recommended that when you are able to walk briskly for about 400 yards and are comfortable performing an emergency stop, you can start driving. This is usually about three to six weeks after surgery (unless you are told otherwise by Mr Khazim or your physiotherapist). If possible take your first drive on quiet roads. You will need to adjust your seat to ensure you are maintaining a good posture throughout your journey. Start with short journeys of no more than 20-30 minutes and gradually increase the length. Break up longer journeys with frequent stops (every 30 minutes), so you can get out and move around for few minutes.
5. When can I travel by plane after surgery?
Although you can travel immediately after surgery, we advise, whenever possible, to avoid short flights for 6 weeks and long-haul flights for 12 weeks after surgery. This is to 1) minimise the risk of developing deep venous thrombosis and pulmonary embolus, 2) decrease low back pain which is particularly worse on sitting after lumbar discectomy and fusion and 3) allow initial physiotherapy treatments and advice before travelling.
Whenever possible, it is advised to have extra leg room while travelling and to change position from sitting every 20-30 minutes to get up and move around for few minutes.
6. When can I commence exercises after surgery?
While in hospital after surgery, you will be reviewed by an experienced physiotherapist who will advise you about post-surgical activities and exercises. The physiotherapist will be happy to answer your questions.
You will have a course of physiotherapy for several weeks and up to 3 months after surgery. You will be seen by an experienced physiotherapist with the aim of gaining full range of motion, strength, and flexibility to maximize your physical and emotional recovery after surgery.
Commencing exercises after surgery varies depending on your general health, fitness, your preoperative condition and limitations and the particular operation you had. Usually, you will have an appointment with an experienced physiotherapist within a couple of weeks and by Mr Khazim about 4-6 weeks after surgery. You should not participate in any sporting or other activity except as advised by the physiotherapist or Mr Khazim. The list below is a guide to the approximate length of time until you may return to sporting activities. Should you wish to commence any other activities, please discuss them with the physiotherapist or Mr Khazim.
| Sport | Lumbar Decompression or Microdiscectomy procedures | Lumbar fusion +/- Decompression |
Cervical discectomy & disc replacement or fusion |
|---|---|---|---|
| Pilates | 6+ weeks | 8-12 weeks | 8 weeks |
| Yoga | 8+ weeks | 12 weeks | 12 weeks |
| Swimming (not Breast Stroke) | 6 weeks | 6 weeks | 6 weeks |
| Light gym weights |
8+ weeks | 10+ weeks | 8+ for Disc replacement 10+ weeks for fusion |
| Static cycling | 6 weeks | 6-8 weeks | 6-8 weeks |
| Normal cycling | 9 weeks | 12 weeks | 12 weeks |
| Tennis, Running, Badminton, Golf or contact sports | 3+ months | 3+ months | 3 months |
7. When can I do my domestic activities after surgery?
Commencing domestic activities after surgery varies depending on your general health, fitness, your preoperative condition and limitations and the particular operation you had. The list below is a guide to the approximate length of time until you may return to doing those activities. Should you wish to commence any other activities, please discuss them with the physiotherapist or Mr Khazim.
| Activity | Lumbar Decompression or Microdiscectomy procedures | Lumbar fusion +/- Decompression |
Cervical discectomy & disc replacement or fusion |
|---|---|---|---|
| Shopping | 4-6 weeks | 4-6 weeks | 6 weeks |
| Cooking | 4-6 weeks | 4-6 weeks | 6 weeks |
| Ironing | 8 weeks | 8 weeks | 6 weeks |
| Vacuuming | 8 weeks | 10-12 weeks | 10 weeks |
| Making the bed | 6 weeks | 6 weeks | 6 weeks |
| Washing/hanging clothes |
8 weeks | 8 weeks | 6 weeks |
| Mopping/sweeping | 8 weeks | 8 weeks | 6 weeks |
| Cleaning bathroom/bath | 8 weeks | 8 weeks | 6 weeks |
| Reaching high/low cupboards |
8 weeks | 8 weeks | 6 weeks |
| Gardening | 3 months | 3 months | 3 months |
8. Functional activities (Walking, Bending, Lifting,…)
Walking: It is important to maintain your mobility and fitness. The distance you will be able to walk varies from person to person. You will not injure your spine by walking, so long as you maintain a good posture. If your walking has previously been limited, it is best to increase the distance and speed gradually. Always maintain a comfortable level of activity.
Bending: Bend your hips and knees, not your back.
Lifting: Do not lift heavy objects and always bend your knees/hips to pick up objects. When lifting, tighten your tummy muscles before you lift and keep them tightened. Know your limits, lift what you are able to manage and ask for help as necessary. Reduce the load where possible into several smaller loads. When carrying an object, keep it close to your body.

Twisting: Avoid twisting; instead, turn the whole body by moving your feet. Reaching: Rearrange your work area, avoid reaching and make sure commonly used items are close by. Avoid lifting arms above shoulder height.
Pushing/pulling: Tighten your tummy muscles first.
Sleeping:
Lying: You should lie either on your back or on your side. Whilst lying on your back, a pillow under your knees may help to relieve pressure on your lower back. If lying on your side you should always have a pillow between your knees. A pillow under your waist may also be helpful.

Turning in bed: You should ‘log-roll’ at all times. Bend your knees up, bringing one leg up at a time. Keeping your knees in line with your body, reach across with your arm and then roll using your knees and shoulders at the same time to avoid twisting in the middle.
Lying to Sitting: Once you have log-rolled onto your side, drop your feet over the side of the bed and at the same time push up with your arms to sit up.

Sitting: Initially you will have to slowly increase the length of time you spend sitting. Start by sitting in a chair, with good posture, for no longer that 20 minutes. If you feel uncomfortable before time has elapsed you should go back to bed. Your sitting time should increase slowly, as you feel comfortable. Whilst sitting, you should try to maintain the natural curve of your spine. Keep your feet flat on the floor with your hips and knees bent at 90 degrees; you will need a supportive chair which is the right height to allow you to do this.

Mobility/Walking: Whilst walking, you should maintain a good posture at all times and should not need any walking aids. Initially after the operation you will walk with the support of one or two staff as necessary. The use of walking aids is not advised as they encourage you to lean forward and adopt a poor posture. Mobilise as tolerated and increase as able.
Stairs: Use the banister for balance. If one leg is stronger and less painful, lead with this leg going upstairs and take one step at a time. To go downstairs, put the weaker/more painful leg down first.
Washing, Showering and Dressing Advice:
Dressing the Lower Half of the Body - there are several techniques:
- Standing, keep your back straight, place one foot at a time on a chair.
- sitting, bring one leg up at a time, resting ankle on the knee.
- Lying on the bed, bring one foot up at a time. The physiotherapist may be able to offer other helpful information.
Washing, Brushing Teeth and Hair Washing - all involve leaning forward. Try to maintain your natural curve by these methods: No bathing, take showers only If your basin is next to the bath, sit on the edge of the bath to brush your teeth. If not, then try a stool in front of the basin. When standing at the basin, bend your knees to lower yourself. Wash your hair by kneeling by the side of the bath and tilting your head forward. You will need a showerhead or jug to rinse. Try a folded towel to pad the edge as you lean over the bath. Sit in a chair leaning back over a sink as you would at the hairdressers if someone else is available to help. A reclining patio chair is useful to get a good position. Or a couple of folded towels will give support to the lumbar spine yet enable good positioning for washing.
Sex: As a general rule you should take a passive role, normally lying on your back. Try to avoid bending and twisting your spine.
TV/ Cinema: Maintain your natural curve when watching TV or in the cinema. Take frequent breaks and do not stay in one position for more than 20-30 minutes.
Pacing: This is the way to increase your activity level in spite of the pain, thus achieving your own personal goals. Start by deciding what your current level of comfortable activity is (your base line), that is the number of repetitions of an exercise, e.g. walking distance, sitting time, number of step ups or each exercise. Increase the activity in a gradual, controlled manner every day or every other day. This will prevent you from overdoing it.
9. General Postural Advice
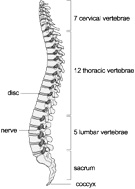
When viewing the human spine from the side we have a natural s-shaped curve in our back. This is the natural positioning of the spine and should be maintained as much as possible during standing, sitting or lying. If you assume a prolonged slumped or flexed (bent forwards) posture this may increase your spinal problems and cause pain. Try to promote the natural curve by tucking your bottom under, bringing your shoulders back into alignment and tightening your tummy muscles.
10. Postoperative Physiotherapy and Exercises
Before leaving hospital after spinal surgery (not spinal injections), you will be given an appointment for outpatient physiotherapy within a couple of weeks. You will be seen by a senior experienced physiotherapist who will assess you and answer any questions you may have about activities. An exercises and activities programme will be planned with the aim of gaining full range of motion, strength, and flexibility to maximize your physical and emotional recovery after surgery. If there are any concerns, the physiotherapist may arrange for a review by the resident medical officer or Mr Khazim.
The exercises that you will be asked to do should not hurt. They should be performed gently with low effort.
- Relax and breathe comfortably during all exercises.
- When exercising, try to relax the muscles of your arms and neck.
- Do not exercise into pain.
- If any exercise increases your pain or makes the pain worse after completion, try decreasing the number of repetitions and the intensity at which you perform them.
- Use your hands to feel the muscles you need to keep tight. This may help you to become more aware of the correct muscles which hold your spine in a good position.
- Always perform exercises slowly and rhythmically.
- If you are tired and having trouble controlling your movements, relax and try again later.
